Neuro-Ophthalmology
- Services
- Neuro-Ophthalmology
OPTIC NERVE
The optic nerve is a critical link between the eye and the brain, transmitting visual information for interpretation. Comprised of over a million nerve fibers, it plays a central role in visual processing. Damage to the optic nerve can result in vision loss and other visual impairments. Understanding the optic nerve's anatomy is crucial in diagnosing and managing various eye conditions and neurological disorders. Empowering patients with knowledge about the optic nerve can facilitate early detection and treatment of related issues, promoting better eye health and visual outcomes.

World Class Investigations That Can Diagnose Various Neurological Disorders
Several advanced machines and technologies are used in the diagnosis of neuro-ophthalmic diseases to assess various aspects of visual function and neurological health. Some common diagnostic tools and machines include:
1. Optical Coherence Tomography (OCT) & OCT-Angiography
This non-invasive imaging technique uses light waves to create cross-sectional images of the retina, optic nerve head, and other structures at a microscopic level, aiding in the assessment of conditions like optic neuritis, optic nerve atrophy, and other neuro-ophthalmic disorders. Additionally, OCT angiography helps in diagnosing and monitoring ischemic optic neuropathy that occurs in diabetic and hypertensive patients.
2. Visual Field Testing
Performed using devices such as automated perimetry machines like the Visual Field Analyzer, this test evaluates the full horizontal and vertical range of vision to detect abnormalities caused by conditions such as optic nerve damage, pituitary tumors, and other neurological disorders.
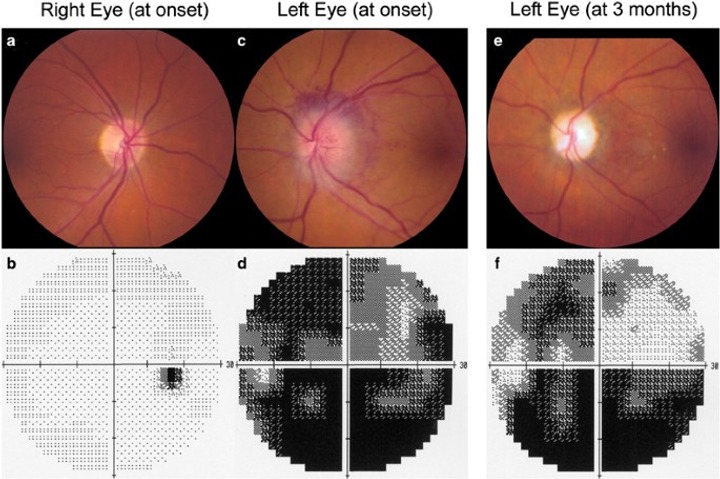
3. Sequential Fundus Photography
This imaging technique captures detailed images of the back of the eye, including the optic nerve, retina, and blood vessels, helping to document and monitor changes associated with neuro-ophthalmic conditions like papilledema, optic nerve drusen, and diabetic retinopathy.

Optic Neuritis
What is Optic Neuritis?
Optic neuritis is an inflammation of the optic nerve, the nerve that connects your eye to your brain. This nerve is essential for vision because it carries visual information from your eye to your brain, allowing you to see.
Symptoms to Look Out For:
Vision Loss
You might notice a sudden decrease in vision in one eye. This can range from mild blurring to severe loss of vision.
Pain
Often, there is pain in the affected eye, especially when you move it.
Color Vision Changes
Colors might appear less vibrant or washed out.
Flashing Lights
Some people report seeing flashing lights or flickers.
What Causes Optic Neuritis?
The exact cause of optic neuritis isn't always clear, but several factors can contribute to its development:
Autoimmune Diseases
Conditions like multiple sclerosis (MS) are common culprits. In MS, the immune system mistakenly attacks the optic nerve.
Infections
Certain viral or bacterial infections can lead to optic neuritis.
Other Diseases
Conditions such as lupus or sarcoidosis can also cause inflammation of the optic nerve.
Medications and Vaccinations
In rare cases, certain medications or vaccines can trigger optic neuritis.
How is Optic Neuritis Treated?
Steroids
The main treatment for optic neuritis is corticosteroids, which reduce inflammation. These are usually given through an IV (intravenous) for a few days, followed by oral steroids.
Plasma Exchange Therapy
If steroids aren't effective, this procedure, which involves replacing the plasma in your blood, might be used.
Managing Underlying Conditions
If an autoimmune disease like Multiple Sclerosis is the cause, treatment will focus on managing that condition.
Recovery Support
Vision often starts to improve on its own within a few weeks to months. Your doctor will monitor your recovery and may suggest specific rehabilitation exercises or therapies to support your vision.
Living with Optic Neuritis
Regular Check-ups
It's essential to have regular follow-ups with your eye doctor or neurologist.
Healthy Lifestyle
Maintaining a healthy diet, exercising, and managing stress can support your overall health.
Support Groups
Connecting with others who have experienced optic neuritis can provide emotional support and practical advice.
Optic neuritis can be a scary experience, but with proper medical care and support, many people recover well. If you have any symptoms or concerns, it's important to seek medical attention promptly.

IIH (Idiopathic Intracranial Hypertension)
What is Idiopathic Intracranial Hypertension?
Idiopathic intracranial hypertension (IIH) is a condition where there is increased pressure around your brain without a clear cause. The increased pressure can cause headaches and vision problems. "Idiopathic" means the cause is unknown, and "intracranial" means within the skull.
Symptoms to Look Out For:
Headaches
Often, these are severe and can feel similar to migraines. They might be worse in the morning or when you bend over.
Vision Problems
This can include blurred or double vision, brief episodes of blindness in one or both eyes, and seeing flashing lights.
Tinnitus
Some people hear a "whooshing" sound in their ears that matches their heartbeat.
Nausea and Vomiting
Feeling sick to your stomach and vomiting can also occur due to the increased pressure.
What Causes Idiopathic Intracranial Hypertension?
The exact cause of IIH is unknown, but several factors might increase the risk, including:
Obesity
Being overweight is a significant risk factor.
Medications
Certain medications, such as those used for acne or tetracycline antibiotics, might contribute.
Hormonal Changes
Changes in hormones, such as those during pregnancy or from taking birth control pills, can play a role.
How is Idiopathic Intracranial Hypertension Treated?
Medications
Drugs like acetazolamide can help reduce the production of cerebrospinal fluid, thereby lowering pressure. Sometimes, diuretics (water pills) are also used.
Weight Loss
If you are overweight, losing weight can significantly reduce symptoms and lower pressure.
Therapeutic Procedures
In severe cases, procedures like a lumbar puncture (spinal tap) can relieve pressure temporarily. Surgery might be considered if other treatments are not effective.
Regular Monitoring
Regular eye exams and visits to your doctor are crucial to monitor and manage vision changes and pressure levels.
Ocular Nerve Paralysis
What is Ocular Nerve Palsy?
Ocular nerve palsy refers to a condition where one or more of the nerves controlling the muscles around the eye become impaired, leading to issues with eye movement and alignment. The main nerves involved include the oculomotor nerve (III), trochlear nerve (IV), and abducens nerve (VI).
Symptoms to Look Out For:
Double Vision (Diplopia)
Seeing two images of a single object.
Eye Misalignment
One eye may turn inward, outward, upward, or downward.
Difficulty Moving the Eye
Trouble moving the eye in certain directions.
Drooping Eyelid (Ptosis)
The eyelid on the affected side may droop.
Pupil Changes
Changes in pupil size or reaction to light, especially with oculomotor nerve palsy.
How is Ocular Nerve Palsy Diagnosed?
Medical History and Physical Examination
Your doctor will ask about your symptoms and medical history, and then conduct a physical exam to check for eye movement and alignment issues.
Neurological Examination
This exam assesses nerve function and helps determine which nerve is affected.
Imaging Tests
MRI or CT Scans to identify any abnormalities like tumors, aneurysms, or lesions pressing on the nerve.
Blood Tests
To check for underlying conditions such as diabetes, infections, or autoimmune diseases.
Lumbar Puncture (Spinal Tap)
In some cases, this test may be used to check for infections or inflammation in the cerebrospinal fluid.
How is Ocular Nerve Palsy Treated?
Medications
Steroids to reduce inflammation and swelling. Antibiotics or antivirals if an infection is the cause. Pain relievers to manage any associated pain.
Surgery
Decompression surgery to relieve pressure on the nerve from a tumor, cyst, or aneurysm. Strabismus surgery to realign the eyes if double vision persists.
Eye Patching or Prisms
Temporarily covering one eye can help manage double vision. Prism glasses can help align the images seen by the two eyes, reducing double vision.
Physical Therapy
Eye exercises to improve coordination and strengthen the eye muscles.
Treating Underlying Conditions
Managing diabetes, hypertension, or other systemic conditions contributing to the nerve palsy.
Living with Ocular Nerve Palsy
Regular Follow-ups
Continuous follow-up with your eye doctor is crucial to monitor recovery and adjust treatments as needed.
Healthy Lifestyle
Maintaining a balanced diet, exercising, and managing stress can support your overall well-being.
Support Networks
Connecting with others who have ocular nerve palsy through support groups can provide emotional support and practical.
Adaptations
Making adjustments in your daily life, such as using assistive devices or modifying activities, can help manage symptoms and improve your quality of life.
Ocular nerve palsy can be a challenging condition, but with the right diagnosis, treatment, and support, many people manage their symptoms effectively and lead fulfilling lives. If you experience symptoms or have concerns, seek medical attention to explore the best treatment options for your situation.

Ischemic Optic Neuropathy
AION (Arteritic Anterior Ischemic Optic Neuropathy) and NAION (Non-Arteritic Anterior Ischemic Optic Neuropathy) are conditions that affect the optic nerve, leading to sudden vision loss. They differ mainly in their underlying causes and treatments.
Symptoms to Look Out For:
Sudden Vision Loss
Both conditions typically cause a sudden, painless loss of vision in one eye.
Visual Field Defects
There may be areas of vision that are missing, often noticed as dark spots or shadows.
Swollen Optic Disc
An eye examination may reveal swelling of the optic disc, where the optic nerve enters the eye.
Color Vision Changes
Colors may appear less vibrant or faded.
AAION (Arteritic Anterior Ischemic Optic Neuropathy)
Causes: Giant Cell Arteritis (GCA): This is an inflammation of the blood vessels (arteries), which can restrict blood flow to the optic nerve, leading to vision loss. It primarily affects older adults.
Diagnosis: Blood Tests: Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels indicate inflammation. Temporal Artery Biopsy: A sample of the artery is taken to confirm the diagnosis of GCA. Clinical Examination: Symptoms such as scalp tenderness, jaw pain, and fever may support the diagnosis.
Treatment: Steroids: High-dose corticosteroids are immediately started to reduce inflammation and prevent further vision loss. Monitoring: Regular follow-up is necessary to adjust steroid dosage and monitor for side effects.
NAION (Non-Arteritic Anterior Ischemic Optic Neuropathy)
Causes: Small Vessel Disease: Poor blood flow to the optic nerve due to conditions like diabetes, high blood pressure, or sleep apnea. Optic Disc Structure: A crowded optic disc can increase the risk, often found in people with a "disc at risk."
Diagnosis: Clinical Examination: Assessment of vision, optic disc appearance, and medical history. Imaging Tests: Optical coherence tomography (OCT) can help visualize the optic nerve and surrounding structures. Blood Tests: To check for underlying conditions like diabetes or high cholesterol.
Treatment: Managing Underlying Conditions: Controlling blood pressure, blood sugar, and cholesterol levels. Lifestyle Changes: Quitting smoking, maintaining a healthy weight, and treating sleep apnea. Vision Aids: If vision loss persists, low vision aids and rehabilitation can help maximize remaining vision.
AAION and NAION can be challenging conditions, but with the right diagnosis, treatment, and support, many people manage their symptoms effectively and maintain a good quality of life. If you experience symptoms or have concerns, seek medical attention to explore the best treatment options for your situation.
Why Choose AcuraVision for Neuro-Ophthalmology?
- Specialized neuro-ophthalmologists with dual training in neurology and ophthalmology
- World-class diagnostic capabilities including OCT, OCT-Angiography, Visual Field Testing, and Sequential Fundus Photography
- Comprehensive evaluation and treatment of complex neuro-ophthalmic conditions
- Advanced imaging coordination with radiology for MRI and CT scans
- Collaborative approach with neurology and neurosurgery teams
- Personalized treatment plans for each patient's unique condition
